Managing Depression in Patients with Chronic Kidney Disease to Slow Progression
New research is further demonstrating the link between depression and progression of kidney disease. A value-based approach to depression screening and treatment is critical to improving patient outcomes.
tags

A new data analysis by Interwell Health suggests that identifying depression in people living with chronic kidney disease (CKD) through annual screenings, which enables proper follow-up and treatment, can improve overall well-being, slow disease progression, reduce hospitalizations, and lower the total cost of care
In a review of 1,561 Interwell patients identified with signs of moderate to severe depressive symptoms in 2022, more than 71 percent (1,111) improved to mild or no depressive symptoms during a subsequent screening.
“This finding further demonstrates that our value-based approach to screening and treatment for all our patients experiencing depressive symptoms is critical to our work to improve patient outcomes,” said Jessica Demaline, senior vice president of healthcare operations at Interwell and a licensed social worker. “The evidence is growing that we must address depression and other behavioral health concerns as a first step to caring for people with kidney disease.”
Prevalence of depression in CKD
Patients with kidney disease experience depression at significantly higher rates than the general population, with an average prevalence rate that ranges between 20 and 30 percent.1
A study in Kidney International concluded that the prevalence of depression is “3 to 4 times higher in patients with CKD... compared with the general population and 2 to 3 times higher compared to individuals with other chronic illnesses.”1
In an analysis of almost 30,000 patients cared for by Interwell who completed a PHQ-9 depression screening test in 2022, we observed that 27 percent reported signs of at least mild depressive symptoms, while 8 percent reported signs of moderate or severe depressive symptoms.
"If patients do not address their emotional health, they are not going to feel motivated to take care of their physical health." - Kasey Bosco, licensed social worker and clinical operations manager
Linking depression and progression
Addressing depression in patients with chronic kidney disease (CKD) has been the subject of increasing research given its impact on overall health. Recent studies suggest that patients living with depression and CKD have a statistically higher risk of disease progression and hospitalization.
A 2023 study examined data from more than 150,000 patients and found an association with disease progression, defined as a loss of kidney function of more than 40 percent (as measured by eGFR).2
“Our study yielded significant estimates for three single kidney outcomes that manifest different degrees of disease progression,” wrote authors Dr. Nanbo Zhu and colleagues in the Clinical Kidney Journal.
For those diagnosed with depression, the researchers observed a 38 percent increase in the rate of kidney function decline, 32 percent higher rate of replacement therapy such as dialysis, and an 84 percent higher mortality rate.
The authors suggested several explanations for the associations observed in their study including a possible relationship to inflammatory and immune–metabolic pathways, the associated higher risks of cardiovascular and cerebrovascular disease with depression, and changes in social, lifestyle, and medical behaviors, which can accelerate decline in kidney function.
A separate 2023 study in the International Journal of Cardiology supported this conclusion, finding that patients with CKD and depression are almost 30 percent more likely to develop cardiovascular disease.3
The PHQ-9 depression screening test
The identification of depression is the first step to implementing changes that can alleviate those symptoms. An effective value-based program offers patients support from social workers, nurses, and dietitians who educate and empower them to better manage their kidney disease and other diagnoses such as depression.
"If patients do not address their emotional health, they are not going to feel motivated to take care of their physical health,” said Kasey Bosco, a licensed social worker and clinical operations manager for Interwell who leads a team of nurses providing depression screenings. “When patients face clinical depression, they are more likely to experience social isolation. The result can be an inability for patients to properly manage their kidney disease and other chronic conditions.”
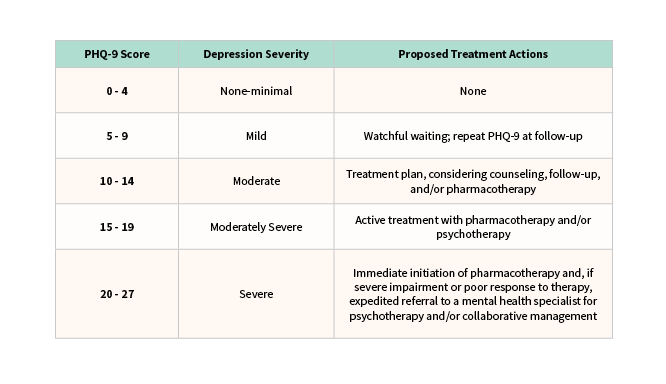
The PHQ-9 screening, first established about 20 years ago, is a highly effective and well-established series of questions that can identify early signs of depression.4 The screening tool is used by Interwell’s care team and conducted for patients on at least an annual basis. The resulting score from 0 to 27 falls into these categories with suggested recommendations for intervention.5
After a score of 10 or above (moderate to severe depressive symptoms), or if the Interwell care team determines the symptoms are impacting a patient’s quality of life, then the team takes a series of follow-up steps which include:
- Reviewing results with the patient
- Partnering with the patient and provider to create an individualized plan
- Referring the patient to their social worker, mental health provider, or primary care doctor
- Addressing any social determinants of health issues (such as food insecurity, housing instability, and transportation challenges) that can impact wellbeing
- Discussing medication management with the appropriate provider
Implementation and Impact
One Interwell patient described the impact of a kidney disease diagnosis like this: “Sometimes you feel like your family doesn't understand because they don't. They can sympathize but don't understand. You feel alone and that causes depression.”
This patient worked with Interwell’s team of social workers, nurses, and dietitians for over a year, providing her support, empathy, and encouragement. This resulted in major changes to her diet and exercise, a more positive outlook, and a pre-emptive transplant.
"The lack of diagnosis and a good test for screening had been a real challenge," said Dr. Nauman Shahid of Eastern Nephrology Associates in North Carolina. “Better depression screening in value-based care programs is helping us diagnose a lot of patients who would otherwise go undiagnosed for a long period of time.”
Interwell embeds renal care coordinators (RCCs) in Dr. Shahid’s nephrology practice, and one of the first steps for all patients is screening for depressive symptoms. In one case, the RCC administered a PHQ-9 screening to a patient who received a score of 25 on their PHQ-9, a sign of severe depressive symptoms. In working with her nephrologist and Interwell care team, the score fell to 12 in less than a year.
Because Eastern Nephrology is in a rural area, outside behavioral health resources are often not available. Nephrologists instead follow treatment guidelines designed in partnership with Interwell to help them better support patients with depressive symptoms.
“The resources for depression screening and treatment we developed with the help of Interwell were very helpful,” said Dr. Shahid. “Most nephrologists and advanced practice providers are now comfortable diagnosing and treating depression. That can make a big difference for our patients’ overall health.”
Interwell continues to strengthen its work around depression screening and intervention protocols to support even more patients and improve outcomes.
References:
Shirazian S, Grant CD, Aina O, Mattana J, Khorassani F, Ricardo AC. Depression in Chronic Kidney Disease and End-Stage Renal Disease: Similarities and Differences in Diagnosis, Epidemiology, and Management. Kidney Int Rep. 2016 Sep 20;2(1):94-107. doi: 10.1016/j.ekir.2016.09.005. PMID: 29318209; PMCID: PMC5720531.
Nanbo Zhu, Suvi Virtanen, Hong Xu, Juan Jesús Carrero, Zheng Chang, Association between incident depression and clinical outcomes in patients with chronic kidney disease, Clinical Kidney Journal, Volume 16, Issue 11, November 2023, Pages 2243–2253, https://doi.org/10.1093/ckj/sfad127
D'Oro A, Patel DH, Wass S, Dolber T, Nasir K, Dobre M, Rahman M, Al-Kindi S. Depression and incident cardiovascular disease among patients with chronic kidney disease. Int J Cardiol Cardiovasc Risk Prev. 2023 Jul 18;18:200199. doi: 10.1016/j.ijcrp.2023.200199. PMID: 37534371; PMCID: PMC10391655 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10391655/
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606-13. doi: 10.1046/j.1525-1497.2001.016009606.x. PMID: 11556941; PMCID: PMC1495268. https://pubmed.ncbi.nlm.nih.gov/11556941/
From Kroenke K, Spitzer RL, Psychiatric Annals 2002;32:509-521 https://jacobimed.org/public/Ambulatory_files/mlove/CurriculumWomenandGeri/Depression/Depression%20articles/PHQ-9ReviewKroenke.pdf